Event
Why Integrations Matter for Clinical Communication
Watch NowTABLE OF CONTENTS
Burnout has become a point of concern in nearly every industry, and healthcare workers are at the forefront of the discussion. Physicians, clinicians, residents, and even administrators across the healthcare industry are tired, and it’s time to find actionable ways to minimize the impact of burnout. This is especially important for those who are newer to the healthcare workforce. Grueling work hours have long been a part of medical training, but thankfully, conversations about burnout have fostered positive change. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) limited working hours for residents to 80 hours per week with shifts no longer than 24 consecutive hours.1 Prior to that, “resident physicians routinely worked 90–100 hours per week, for up to 36 consecutive hours without rest, for the entire duration of residency training.”2
So, how can academic healthcare organizations meet ACGME’s regulations and reduce burnout while maintaining exceptional patient experiences? While addressing hours worked was a great place to start, almost two decades later, more can be done to enhance speed to care while giving residents more freedom and flexibility with their schedules. That’s where modern technology steps in to take care of crucial elements—such as schedule creation—to allow residents to focus on what they want to do most: learn how to save lives.
Because residents have so much on their plate, balancing shifts is essential to fighting burnout. We’ll look at five ways better scheduling improves resident satisfaction:
Setting scheduling rules that limit weekly work hours to ensure fair shift distribution should be a top priority. In academic medicine, meeting the 80-hour work week guidelines is even more difficult than it seems. A multitude of scheduling factors—including physicians’ teaching requirements, research duties, and clinical responsibilities—must be considered. As a result, it can be difficult to manually prioritize work limits and shift equity with other scheduling rules.
An advanced scheduling solution can easily accommodate complex scheduling variables once rules are set to limit work hours and balance providers’ varying responsibilities. What’s more, the system should also have the ability to factor in providers’ preferences and ensure that certain shifts, like weekends, nights, and on-calls, are distributed among providers as evenly as possible.
Though this sounds complex, it’s an essential part of balancing a resident’s schedule and, in turn, fighting burnout. The right provider scheduling solution will simplify this process and help improve outcomes for academic healthcare organizations.
When you have a solution that centralizes real-time schedules in a single location, you increase schedule visibility and transparency. Creating schedules is one thing, but ensuring providers can access the latest schedule is another issue. Locating an up-to-date schedule can be a huge source of frustration for providers, and it can also have a big impact on patient care. An advanced scheduling solution makes the latest schedules from across your organization accessible to providers at any time from any device in any location.
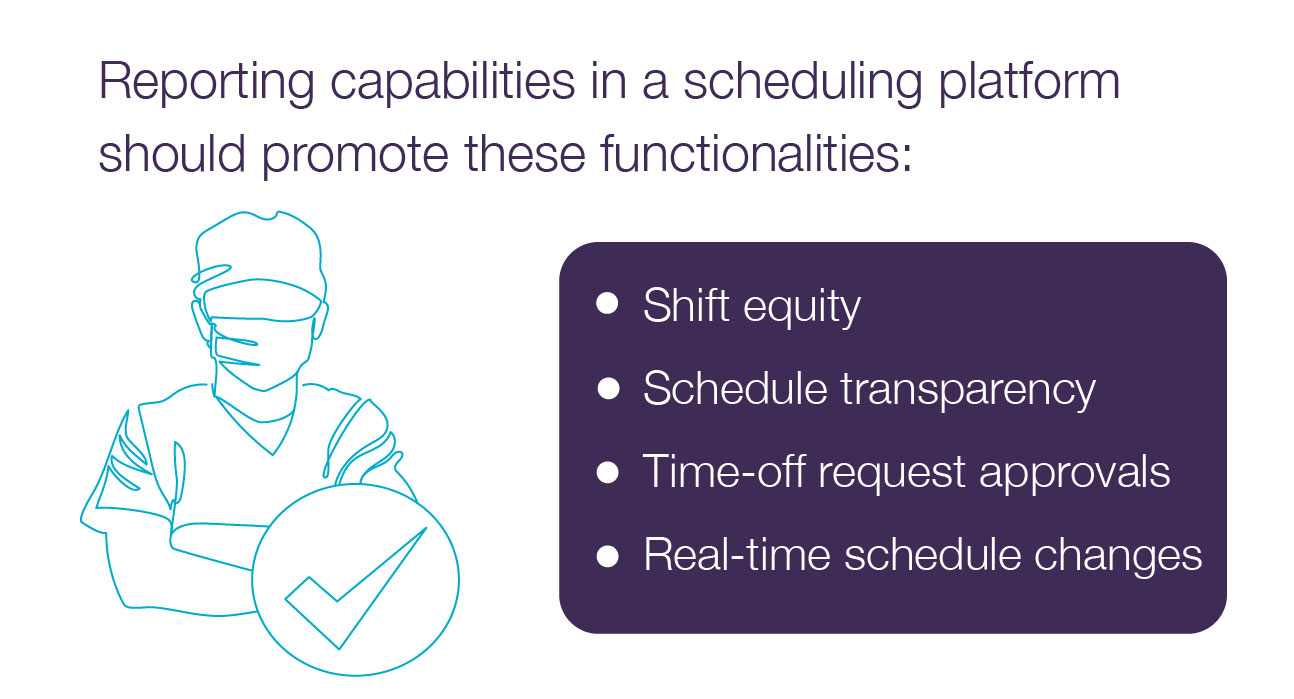
The ability to easily view schedules across devices cuts down on frustration by making it simpler to find and contact the on-call provider and communicate with colleagues. It also increases visibility into the schedule creation process. For example, if a resident goes on their mobile app to request Friday off and sees that two other team members have already requested that day off, it may be less surprising if the request is denied. The reporting capabilities available in the scheduling platform should also promote transparency by allowing schedulers to share reports around shift equity, approval of time-off requests, and more.
When residents want to swap shifts or request time off, the process should not be arduous or overly complex. Just as transparency in other users’ schedules eases frustration, the ability to ask for schedule changes easily enhances the provider experience.
The lack of a simple, standardized process for shift swapping and time-off requests can make it unnecessarily challenging to find the right person to take over a shift when needed. It can also lead residents to swap shifts without letting the proper administrators know, resulting in outdated, inaccurate schedules that delay communication and patient care.
Centralizing time-off requests, shift swapping, and other scheduling requests on a single digital scheduling platform puts the schedule back into the provider’s hands, giving them more autonomy and control over how and when they are scheduled without leaving administrators in the dark.
Time is one of the most important factors in a physician’s day-to-day job, and knowing what’s coming today, tomorrow, and even next month will help residents be as prepared as possible. This is why schedules should be widely and easily accessible, and auto-generated, real-time updates can enhance that process even more with the right scheduling solution.
Creating schedules can also be incredibly time consuming, especially in academic settings. Schedulers often try to balance teaching, research, and patient care with organizational, departmental, and individual provider needs. Resulting time constraints mean that providers often receive their schedules at the last minute, making work-life balance nearly impossible. But next month’s schedule shouldn’t have to wait until next month!
An advanced scheduling solution can simplify schedule creation with rules built to meet each team’s unique needs. Different departments within an organization can then auto-generate gap-free schedules built to their specifications, which helps administrators complete and distribute schedules much more quickly. Complete schedules should be instantly available for care team members and administrators across the organization to access at any time.
It is essential to free up administrators’ time so they can better support the needs of clinical staff. Roughly 312 hours are spent creating and managing schedules annually per department, and for academic facilities with more complex schedules, the number is likely far higher.3 That’s valuable time administrators (and sometimes providers) could spend finding ways to more effectively support clinical staff.
Loretta Weeks, the Administrative Coordinator for the Division of Hospital Medicine for UNC Hospitals, said PerfectServe Lightning Bolt Scheduling has helped the hospitalist group balance both in-patient and teaching services.
Hear more from Loretta here.
Balancing workloads is essential to fighting the growing challenges of burnout that impact a resident’s work-life balance. The right scheduling solution will create fair and equitable schedules that are transparent, simple to edit, easy to share, and follow ACGME’s guidelines for recommended worked hours.
Lightning Bolt offers optimized schedule creation with the ability to add provider preferences, see shift-swapping opportunities, view real-time changes, and share the most up-to-date and accurate schedule possible. Learn more about Lighting Bolt’s capabilities here.
1,2 Duty Hours and Patient Safety, Agency for Healthcare Research and Quality, Patient Safety Network, Sept. 7, 2019: psnet.ahrq.gov/primer/duty-hours-and-patient-safety
3 The Real Cost of On-Call Scheduling Guide, PerfectServe, 2022:https://www.perfectserve.com/real-cost-on-call-thank-you-page/