How Patient Journey Mapping Improves the Patient Experience
TABLE OF CONTENTS

In the technology-rich world of healthcare, a patient is bound to encounter any number of solutions, tools, and apps throughout their care journey. From a simple prescription refill request to the most complex emergency surgery, providers and clinicians should be able to use these technologies to make every care interaction faster, better, and more satisfying. Too often, siloed solutions cause process breakdowns and communication delays, and it’s not just the care team that suffers.
At a recent Becker’s Healthcare meeting, Miriam Halimi, JD, DNP, MBA, PN-RC, spoke to an audience of healthcare professionals about these common challenges. She walked us through the story of Cynthia, an imaginary patient, to show how healthcare communication technology can ease provider workload and improve patient outcomes throughout their journey.
What is the Patient Journey?
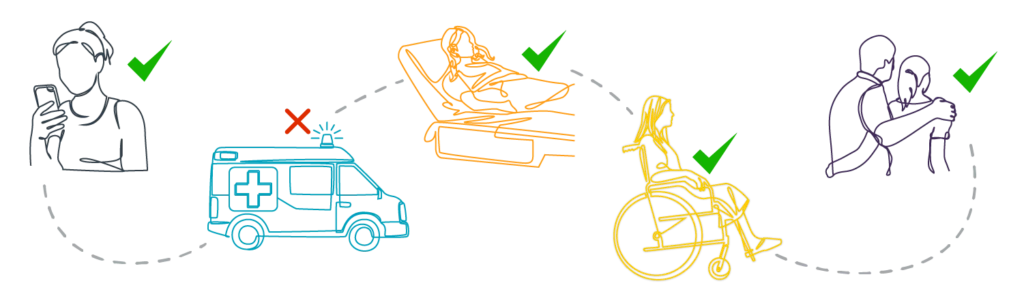
A patient’s journey refers to the elements a patient touches throughout an “episode” of care, with a specific focus on the events from the time care is needed to when post-episode care is concluded.
This includes all the elements that drive care forward: speaking to a provider, initiating an appointment, paying a bill, ordering a prescription, and many more. Examining these aspects of the patient journey is essential to understanding the patient experience.
What is Patient Journey Mapping?
Patient journey mapping is the visual practice of seeing and understanding the relationship between the patient’s journey and their experience. It illustrates how a patient moves through their care journey and affords a better look at the internal and external factors involved in patient satisfaction, care delivery, and care outcomes. In this way, it also details how communication and collaboration among the care team impacts each leg of the patient journey.
Giving providers the tools they need to enhance the patient journey is an essential component of creating a better patient experience. Better tools mean better communication and better provider workflows, which likely leads to better patient outcomes and a more satisfying patient journey.
Connecting the Patient to the Care Team
Our patient Cynthia isn’t feeling great; she’s had progressive abdominal pain all day and now wants to get in touch with her physician. She picks up her phone and calls her clinic, but because the office isn’t open, she’s routed through the organization’s medical answering service.
Dr. Carryl Miller is the primary care physician on call this evening, and Cynthia’s message is quickly routed to him. Using the PerfectServe secure messaging app, he sees Cynthia’s voicemail—which has been transcribed for him to read through—and her callback number. Based on what he reads, he wants to connect with her to speak live. He can of course text or call, but he also has the option to initiate an ad hoc video conference. In a few clicks, he initiates a billable video call to connect with Cynthia.
Cynthia’s phone gets a text message with a link to Dr. Miller’s video call. She doesn’t need a separate app that requires login credentials—she simply taps a link, which launches the video call in her phone’s web browser. Dr. Miller is concerned that Cynthia could be experiencing appendicitis, but he wants her to go to the ED to be sure. Dr. Miller uses his app to locate the ”ED charge nurse” in the directory. After speaking with Dr. Miller, the charge nurse calls one of the emergency physicians working that night and lets them know Cynthia is coming in for an appendectomy workup.
Clear Communication Eases Transitions of Care
The ED physician monitoring Cynthia receives a “Critical Results” alert in his unified PerfectServe inbox: Cynthia’s workup is complete, and it’s confirmed that she has acute appendicitis. The next step is to contact the on-call surgeon, so he goes into the app directory and searches for the “general surgeon on call” and sees Dr. Tran’s name. He messages Dr. Tran that Cynthia is in the ED; she comes down to the ED and admits Cynthia for surgery. Because the app is integrated with the organization’s EHR, when Cynthia is admitted for surgery, Dr. Miller—who initially sent Cynthia to the ED—receives a patient transition notification indicating that Cynthia was admitted. This helps the organization meet one of CMS’s conditions of participation.
Dr. Tran needs to begin surgery, so she puts her app into “Procedure Mode.” This means she doesn’t need to give her personal device to someone in the room to monitor her messages, and she won’t be interrupted or distracted during surgery. If a message comes to Dr. Tran while she’s in surgery, Procedure Mode automatically routes it to the surgical nurse on call, James Toomey. Nurse Toomey is monitoring Dr. Tran’s messages, but Dr. Tran can move out of Procedure Mode whenever she wishes. An incoming trauma alert is sent to Dr. Tran, but it’s routed to Nurse Toomey, who responds that Dr. Tran is in surgery and should be finished in the next 20 minutes or so.
Cynthia is now out of surgery and doing well. Her husband, Lee, who is out of town and couldn’t be present for the surgery, is waiting for an update. Using her app and looking at Cynthia’s patient information, Dr. Tran is able to send Lee a text message to let him know that Cynthia is out of surgery and recovering well. Lee receives the message, but he wants to hear Cynthia’s voice. Because Cynthia doesn’t have her phone, Lee calls the hospital switchboard and asks to speak to Cynthia in her room.
Diego Mendoza works as an operator in the call center. He receives Lee’s call, and using the integrated operator console, he easily locates Cynthia, verifies her information, and connects her to Lee. Importantly, Diego doesn’t need to jump from app to app to connect Lee with his wife. Because all communication workflows are contained within one platform, the process is seamless and efficient.
Collaboration Through Post-Op, Discharge, and Beyond
A while later, Cynthia is feeling thirsty and wants to request water. She presses the Nurse Call button, which is integrated with the facility’s nurse call system and the accompanying pillow speaker in her bed. Her request is routed through PerfectServe to a tech, who works out of the same unified inbox as the nurses on Cynthia’s care team. Patient care tech Jay Fischer receives the alert, and he initiates a call to her pillow speaker to see if she needs anything other than water. Cynthia is all set.
When Cynthia’s nurse Leslie checks on her later, she notices Cynthia’s wound looks a bit abnormal and sends a message to Dr. Tran with an accompanying photo. At the time of the message, Dr. Tran is in surgery. Leslie doesn’t need to try and track down who is covering for Dr. Tran—thanks to the communication platform’s predetermined routing rules, her message is automatically delivered to the next on-call physician, Dr. Deepak Patel. Dr. Patel reviews the image and finds no reason for concern, so he responds to Leslie to say that no further action is needed.
The next morning, Cynthia is progressing well and meeting all the necessary post-procedure benchmarks. Dr. Tran wants to initiate the discharge process and give Cynthia directions for post-discharge care. She looks at Cynthia’s care team inside of her app and finds the care manager assigned to Cynthia’s case. Dr. Tran is also able to set up a video visit later in the day with Cynthia and Lee to go over her discharge plan of care. She enters the discharge orders, which also alerts Dr. Miller—Cynthia’s PCP—that Cynthia is going home.
When Cynthia gets home, she receives an automated text message from the hospital that asks about three things: how well she understood the discharge instructions, her current pain level, and whether or not she filled her prescription. Cynthia wasn’t able to fill her prescription yet, so she answers “no” to the final question. This qualifies as an “aberrant” response—meaning it’s not the desired response—so it is automatically routed to Sue Brady, a patient navigator. Sue uses the communication app to call Cynthia back, and they work together to get Cynthia’s prescription filled as soon as possible. This approach ensures that patients like Cynthia continue to meet important post-discharge milestones to reduce the likelihood of readmission. When problems arise, communication with the provider or a member of the provider’s team can be established quickly to avoid negative outcomes.
How Patient Journey Mapping Can Improve the Patient Experience
By mapping Cynthia’s entire patient journey, the intricacies of her experience become clearer, and any problems that arise can be identified much more easily. With this map, we can see how the constant communication across all members of Cynthia’s care team was a crucial part of each leg of the journey. This affords a clearer glimpse into care issues and other areas that need improvement, which the organization can then use to make changes—or implement better technology—that mitigate problems and boost the patient and provider experience.
By implementing solutions like PerfectServe, a health system provides tools that enhance communication workflows, improve care delivery, and boost the experience for both provider and patient. PerfectServe:
- Creates more reliable workflows that facilitate timely communication across the entire care team.
- Always routes messages accurately and efficiently so that nothing is missed and continuity of care is assured.
- Grants each organization the ability to make unique routing and workflow decisions based on need, staff level, speciality, etc.
- Supports integrations with key clinical, IT, and telecom systems that further improve processes and speed up care delivery.
PerfectServe can become your blueprint for real-time collaboration and improved care delivery. To learn more, download our guide or connect with us today.