Event
From Silos to Synergy: Key Communication Integrations at Roper St. Francis
Register >>TABLE OF CONTENTS
PerfectServe’s Nurses of Note awards program honors those who help us define what it means to be a nurse. They’re selected from a large group of nominees and stand out for their diligence, passion, leadership, and devotion to caring for others.
For the fourth year of the program, PerfectServe is highlighting nurses who have gone a step beyond the rest in their careers. Though we believe all nurses make extraordinary contributions, these honorees stood out to us for their steadfast dedication to the field of nursing, helping to paint a picture of the difference they make for their patients and communities every single day.
In-depth profiles of select winners will be published each month for the rest of the year, so make sure to bookmark our blog to learn more about their stories!
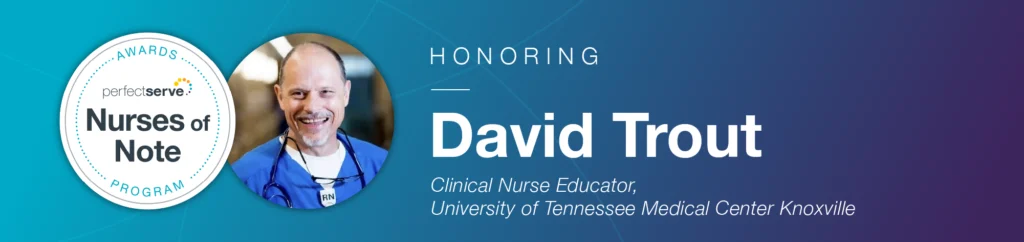
For David Trout, a Clinical Nurse Educator at the University of Tennessee Medical Center (UTMC), his career in nursing was simply meant to be. As a self-described accident-prone child who earned the nickname “Crash,” David spent a lot of time getting care from nurses as a child. He served as a Hospital Corpsman in the Navy, and after some time spent thinking he’d be a doctor, he realized nursing would give him the most time at the bedside. 28 years later, he’s still at it!
David has worked as a nurse at UTMC for nine years but has been in seven different roles since he started. He primarily works as a Critical Resource Nurse (CRN), a role with a primary focus on improving patient safety. CRNs help other nurses solve clinical and critical thinking problems at the bedside in real time, teaching a variety of beside skills such as administering IVs, placing catheters and gastric tubes, equipment troubleshooting, caring for ostomies and other difficult wounds, and more. In short, they focus on rescue, nursing practice, and error prevention.
“We respond to rapid response alerts and codes, facilitate transfers to higher levels of care, and serve as the patient/family advocates at night,” David said. “We have a high percentage of new graduate nurses with limited clinical experience. A lack of experience inherently increases the risk that clinical signs of deterioration may go unnoticed.”
Teaching these skills to new and seasoned nurses alike is part of what David enjoys so much about his role. He’s spent a lot of time reflecting on how to be a better communicator and model best practices in the presence of nursing staff. He’s taken courses and closely examined the outcomes of critical and significant events so he can impart useful knowledge in all care situations.
Though he doesn’t teach physicians or NPs, he does collaborate with them by sharing articles and making recommendations for urgent and emergent care. His nomination stood out to us partly because he created two educational training outlines for care team staff at UTMC. One was about IV tips and tricks, tweaked from a training program he found at a health system in Virginia. For David, it’s all about empowering nurses to take better care of patients.
“It’s important to build trust with staff and to be seen as partners, encouragers, and helpers,” David said.
A large component of David’s role involves technology. Each shift, CRNs use a Sepsis Alert Audit to identify patients at risk of clinical deterioration. David said this program monitors all patients for derangements in selected lab tests and vital signs, and part of his role includes reviewing these programs and assessing at-risk patients. David is also working on an ongoing project with the University Hospitalist Service Nurse Communication Work Group at UTMC to develop a standardized format to help nurses construct high-quality messages using the Situation, Background, Assessment, and Recommendation (SBAR) communication framework. He hopes this will help nurses construct better messages within PerfectServe’s messaging system, which is used by UTMC for clinical communication workflows.
“PerfectServe is an excellent way to communicate, especially since everyone is so accustomed to texting,” David said. “The ability to attach images such as [EKGs and wounds] is very helpful.”
David shared some insight into the many other ways technology has evolved to help nurses deliver better patient care. He specifically shared how much the development of the EHR and computer charting has made patient information more organized and accessible. He’s beginning to try out new tools and software for clinical/pathophysiological questions, evaluations, data tracking, and beyond to explore other avenues where technology can be used to improve nursing as a whole.
“Artificial intelligence offers the prospect of even more robust software that will enhance the early identification of patients at risk for deterioration,” David said. “I am very hopeful for the future of healthcare, particularly as it pertains to the role of AI in research, pharmaceutical development, diagnostics, individualized medication regimens and treatment, telemedicine, and upstream and preventive care.”
On top of being a member of the University Hospitalist Service Nurse Communication Work Group, David serves on the Shared Governance Practice Council and Nursing Peer Review Subcommittee at UTMC. Both teams investigate and evaluate accidents and incidents related to patient care. That’s just one of the other reasons he stood out to us—his devotion to all things communication, nurse empowerment, and patient care are truly noteworthy!
Having been a nurse for over two decades, we also asked David about some of the challenges he sees in nursing today. One of these is nursing attrition, specifically at the bedside. He knows firsthand how hard the work can be and has seen just how much the nursing world has changed since he started in the 90s. He says the pandemic was one of the biggest catalysts for retention issues in the field today.
David has noticed that changes in the field have increased the pool of novice nurses, which isn’t necessarily a bad thing, but it does “create real challenges in delivering excellent care.” He firmly believes longevity in the field establishes a core of experts who can then mentor newer nurses. He hopes the industry can figure out a way to make the bedside more appealing for new talent.
David also thinks that staff across all organizations could benefit from educational programs that teach them how to recognize both existing and potential problems. This could help nurses and all care team staff search for root causes of problems and find solutions, which has a big impact on productivity and safety for providers and patients alike.
As for the industry at large, David hopes decision-makers will utilize shared governance models to ensure staff and leaders are involved in the decision-making process. He speaks highly of the shared governance model in place at UTMC, sharing that it works well because it’s backed by devoted leadership at the organization.
“The value of leaders being present on the front line listening to staff and collaborating to tackle problems together cannot be overstated,” he shared. “When staff feel like they have the clout to effect change, their perceptions of powerlessness will likely be abated.”
David, your dedication to bedside care delivery and nurse education gives us faith in the continued success of the nursing profession. Nurses like you don’t just make a difference in the lives of patients—you also impact the clinicians who work alongside you every day. We’re impressed by your decades-long dedication to the field, and we’re honored to name you a 2024 Nurse of Note!
To learn more about David’s life as a nurse, we asked him a few additional questions:
Why did you choose to become a nurse?
I’ve always been drawn to healthcare. In my twenties, I thought about being a doctor, but after learning more about the roles of doctors and nurses, I realized that nursing would give me the most time at the bedside. It’s my calling!
What is the biggest lesson you learned while serving as a nurse throughout the pandemic?
The pandemic was life-changing for most of us in healthcare. The greatest lesson for me was how innovative and resilient we can be in disastrous situations. Most of us worked extra hours to keep staffing at the safest levels possible. That revealed how dedicated and committed we are as a professional community.
What’s one piece of advice you would give to your younger self about working in the healthcare industry?
I would say to take great care of your physical and mental health.
What do you do to relax after a stressful day?
Spending time with family is the most important thing to me. I also like to walk and read, travel, hang out on the beach, hike, and camp.
What changes would you like to see in the nursing field of the future?
I think there is far too much time spent charting. While I realize charting is necessary for legal and compliance reasons, it seems like we are all nursing the computers more than the patients. The value of clicking the same boxes over and over seems limited at best.
I am hopeful that the future will bring technological and other advancements that improve the quality and relevance of our documentation, freeing us up to get our hands off the keyboards and into the hands of patients.
What’s the biggest life lesson you’ve learned as a nurse?
Most of us will wind up in the hospital at some point, so take care of your patients and family members in the same way you would want to be treated.
Make sure to follow our blog as we publish profiles about more of our amazing Nurses of Note honorees throughout the year!
For more about Nurses of Note 2024, check out the full list of winners.