Event
Why Integrations Matter for Clinical Communication
Watch NowTABLE OF CONTENTS

Nurses are trusted experts who provide incredible patient care. The profession is a calling, a passion, and it is incredibly important that we have the nursing workforce that prioritizes caring for themselves to be fully present for the patients who need them.” – Ryannon Frederick, Chief Nursing Officer, Mayo Clinic, (Becker’s Hospital Review).1
Outdated systems, silos, and disconnected communication among nurses and physicians cause added strain to an already in-demand nursing workforce.2 Nurses can work 9-5 at an acute care facility or they can be seen pushing through 10 to 12-hour rotations. In every situation, nurse communication is a crucial part of their shift, as they are required to share accurate patient information between care providers, in addition to the other responsibilities required of a front-line caregiver for patients and their families.
If they had a list of additional job descriptions and responsibilities, it would include:
Let’s now look at how nurses communicate and balance responsibilities in different contexts.
Imagine you’re in the ED. You have to react moment by moment in the queue as patients pour in, decompensating right in front you. How do you respond? Which patients need care faster? These nurse triage decisions can feel overwhelming.
Now imagine you’re a nurse on the labor and delivery floor. Last-minute emergency C-sections, women rapidly moving through the stages of labor, and patient screams echoing through the hallways. An infant may get rushed and transferred to the NICU for additional neonatal nursing care. It may be an intense, yet rewarding experience when the babies arrive.
Nurses face many different scenarios ranging from geriatric to post surgery care, all while maintaining required documentation demands and changing shift schedules. Nurses have to collaborate quickly and there is a need for communication to be efficient, timely, and reliable. If nurses need to make frequent calls to another care provider, patients may not receive adequate treatment on time.
Imagine this situation at a medical specialist office. They have 2 main clinic locations, and different patient demographics visit each site. Nurses are required at both locations, yet office A is open until 7 PM while office B closes at 5 PM.
It’s 5:10 PM. One patient who regularly visits office B accidentally calls office A from their Google search, thinking they can walk-in to the clinic. The call messaging routes them incorrectly to office A. The covering on-call nurse says it’s okay for them to check in to the office for their chronic condition. However, the on-call nurse doesn’t see in their health record which location this patient usually visits, and there is a lack of notes on file. The nurse waits for a long time, and the patient doesn’t arrive. Frustrated about a lack of provider collaboration and communication, the patient leaves a 1-star review online for the clinic.
The next day, the physician and nurse on-call at site B call site A, disappointed their clinic location received a low patient satisfaction rating. They get the practice owner and manager involved. Now they have a warning discussion with the nurse on-call, when it was truly a breakdown in communication systems for their healthcare clinic.
The physician and nurse collaboration framework in this faux scenario led to poor patient outcomes. In one real-life study, nurses may not always have input or say on how a medical practice is managed. “The participants stated that if nurses were more involved in the development of nursing policies, this would have a positive influence on patient care.”3
Poor communication between clinicians and patients can result in misunderstandings about medications and the miscommunication of follow up instructions, which can result in poor outcomes and readmissions, and could result in a patient coming to harm.4
Whether nurses work for a hospital or private medical practice, better scheduling collaboration and nurse communication software is needed. If nurses are able to find the best communication options for their day-to-day interactions, it would significantly reduce barriers to effective healthcare treatments.
Some nurses said they felt like labourers…if you’re not valued at work, you don’t have the desire to stay in the public system.5
Nurses are in short reserve, but the demand for nurses continues to grow. What can hospitals and group practices do to alleviate their stress? Organizations may increase pay incentives, but is that enough? It’s not just about the money.
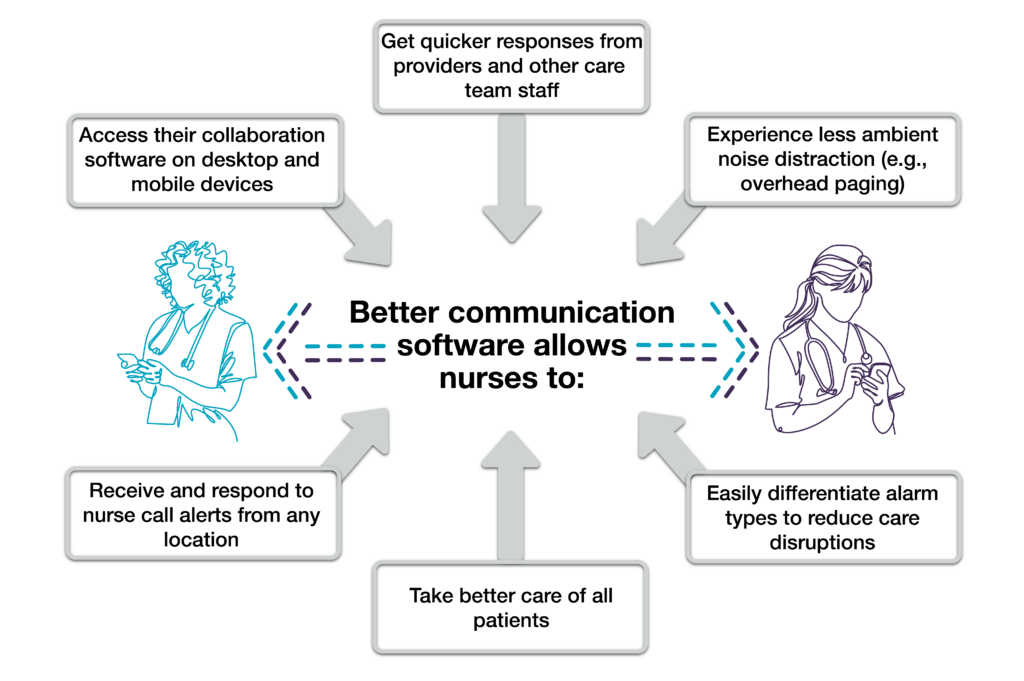
Nurses need a platform to communicate not only the needs of their patients, but for their colleagues as well. Promoting team-based care, sharing of new evidence-based care guidelines, and management of staffing shortages are strategies that leaders can rely on for effective communication platforms. This reduces the burdens experienced by nurses.
With all the roles nurses fill, it’s important for them to communicate in a timely manner. Nurses may leave due to burnout and better pay opportunities,6 and this could result in more miscommunication mistakes among staff. This leads to poor patient outcomes and expensive provider costs. However, there is good news…
When nurses have time to collaborate patient care through text, cell, EHR, or face-to-face, the results improve for patients and providers. Hospital executives and nurse leaders who take time to care for their teams and find appropriate medical communication solutions will create bright spots for the future of nursing.
See how PerfectServe’s Clinical Communication software can eliminate wasted time and help nurses be more efficient.
1Jensik, L. (2021, October 29). Will nurses come back? 3 healthcare leaders weigh in.Becker’s Hospital Review. https://www.beckershospitalreview.com/hospital-management-administration/will-nurses-come-back-3-healthcare-leaders-weigh-in.html
2NursingTimes. https://www.nursingtimes.net/news
3Kieft, R.A., de Brouwer, B.B., Francke, A.L. et al. How nurses and their work environment affect patient experiences of the quality of care: a qualitative study. BMC Health Serv Res 14, 249 (2014). https://doi.org/10.1186/1472-6963-14-249
4Effects of Poor Communication in Healthcare. HIPAA Journal, https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare
5Wilton, K. (2021, September 16). ‘Not about the money’: Nursing report addresses exodus from Quebec’s public sector. Montreal Gazette. https://montrealgazette.com/news/local-news/not-about-the-money-nursing-report-addresses-exodus-from-quebecs-public-sector
6Virkstis, K. (2021, August 12). Why so many nurses are leaving amid delta—and how you can keep them. Advisory Board. https://www.advisory.com/Daily-Briefing/2021/08/12/nurse-shortage#our-take-weve-reached-the-tipping-pointhow-do-organizations-move-forward-see-our-3-keys