Event
Why Integrations Matter for Clinical Communication
Watch NowTABLE OF CONTENTS
In healthcare, “sentinel event” is a widely understood term, and for good reason. The Joint Commission defines a sentinel event as “a patient safety event that results in death, permanent harm, or severe temporary harm,” and further notes that sentinel events “are debilitating to both patients and health care providers involved in the event.”1
No matter the clinical setting, the seriousness with which these events are handled varies only slightly, and the repercussions affect providers, patients, and families alike. When they do occur, a timely response is critical, but wouldn’t it be better if we could reduce the likelihood that they happen at all? The answer to that question is a resounding “yes,” and it turns out that effective clinical communication systems are key to preventing sentinel events before they happen.
To reduce the frequency of sentinel events, you first have to understand what kind of events are happening. Becker’s Hospital Review summarized some of the sentinel events most frequently reported to The Joint Commission for 2021, including:2
These reports were among 1,197 total cases reported to The Joint Commission last year—the highest number reported since the Commission began recording these cases in 2007. With that in mind, it’s apparent that reducing these events should be a top priority, and the outcomes are likely to have wide-ranging benefits for health systems, providers, and patients. So, how does a healthcare system reduce sentinel events using effective communication tools and strategies?
Providers across the care team continuum will almost certainly face alert & alarm fatigue at some point in their careers. Care team members face notification overload during every shift due to excessive alerts, false alarms, and multiple patient monitoring devices competing for their attention. It’s no wonder fatigue sets in when staff can’t easily distinguish between routine alerts and true all-hands-on-deck emergency calls. Alarm fatigue is costly—timely response to critical alarms can be the difference between life and death, but their uniqueness is significantly diluted when all or most alarms sound the same.
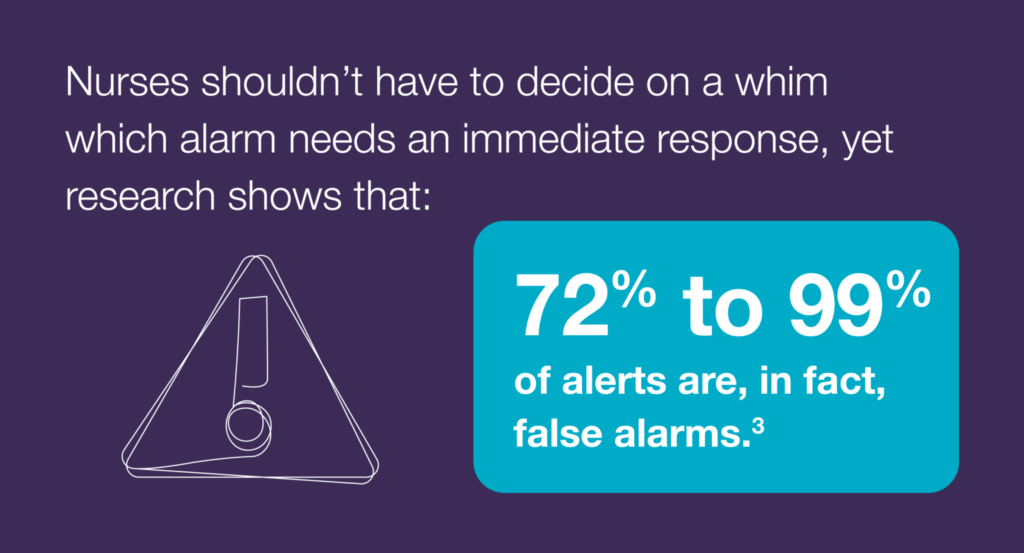
A communication system that can prioritize and manage alerts and notifications accurately addresses alarm fatigue by distinguishing notifications based on event and call type. Solutions that adjust notification sounds based on alert type help the end user understand the nature of the patient event before they even look at their phone or computer. A sentinel event may be altogether avoidable if alarms are properly managed and escalated to the right person with the appropriate level of need. Furthermore, the severity of a sentinel event can be reduced when providers are able to respond to the correct alarm promptly. This is why a clinical communication system that automatically escalates alerts based on severity and notification type can save time, money, and—most importantly—lives. It can even reduce the chance of the event occurring in the first place.
In 2021, another sentinel event, delays in treatment, was reported 97 times. To delay treatment is to delay necessary care, and when failed communication systems cause these delays, hospitals can face serious repercussions, up to and including legal liability. Physicians, nurses, CNAs, and even staff in administrative roles end up dealing with the brunt of these consequences—but they shouldn’t have to. Communication solutions that get critical updates to the right providers at the right time can—and do—alleviate delays in treatment.
Clinical communication systems that are provider- and patient-centered improve speed to care. These systems work to prioritize provider communication and limit distractions, thus mitigating the risk of delaying necessary and life-saving treatment to patients in need. Let’s consider an example. Suppose a surgeon is prepping for a procedure, and they have access to a communication system that automatically reroutes and auto-escalates messages. The communication system is aware of the provider’s schedule, so the surgeon doesn’t have to ask a colleague to cover her. The intelligent solution has already accounted for this scenario, and in this case, the surgeon’s PA might be the first escalation point for urgent calls. All other non-urgent communication would be held until the surgeon is out of the OR, addressing speed to care and limiting any delays to the patient’s treatment. A system that keeps track of which providers are scheduled to be replacements for on-call schedule changes can alert everyone to the change, which limits confusion, prioritizes provider time, and prevents distractions that could inhibit treatment.
To prioritize provider communication is to prioritize patient care. Sentinel events related to medication management can be avoided by using communication tools that prioritize timely, accurate messaging. Communication about medication management is an around-the-clock occurrence—including when patients are sent home from appointments. This is why a clinical communication solution that gets after-hours messages to the right provider or patient is critical. If a patient is discharged, an automated message can be sent to check on the patient after care has been given. The notification system can trigger a follow-up response with a clinical team, such as ensuring medication was filled after a prescription was ordered. By deploying a messaging solution that automatically routes critical information, patients receive their medication on time. This also ensures off-call providers are not interrupted with messages about medication needs, orders, and other patient care tasks—especially important when burnout in healthcare is at an all-time high. While medication management isn’t the most prevalent issue, it does lead to delays in care, provider stress, and patient harm and frustration.
Just as nurses and other care team members can face alarm fatigue, clinical alarm response can bring clinicians to a similar crossroads. Clinical equipment alarms tend to sound similar, and responding to these alarms is tricky since providers usually have to travel back and forth to stationary computers and laptops to acknowledge them. In 2021, 22 sentinel events related to clinical alarm response were reported, but the good news is that it’s possible to significantly reduce these instances when care team members—and specifically nurses—have smartphone-enabled, deeply integrated communication technology at their disposal. This is why many healthcare systems are moving toward smartphone adoption: to accelerate speed to care, and to give nurses the freedom to respond to alerts, messages, and calls from a mobile application. With better nurse communication software, nurses can have the following:
Sentinel events are often costly and distressing, but their frequency can be significantly reduced with the right people, processes, and systems in place. Executives must look at the human and financial impacts sentinel events have on their organizations—and the risk factors that contribute—to understand why a robust clinical communication solution needs to be part of their tech stack. So many aspects of daily patient care are impacted by the ability of care teams to respond efficiently to real-time updates and information, but many organizations still find themselves battling dated and unreliable processes, siloed technology solutions, and the downstream negative effects of these challenges that fall on the shoulders of dedicated-but-overburdened staff. Health system executives should look for communication systems that unify the care team to provide better care, which has further implications for the organization’s ratings, finances, and other patient metrics.
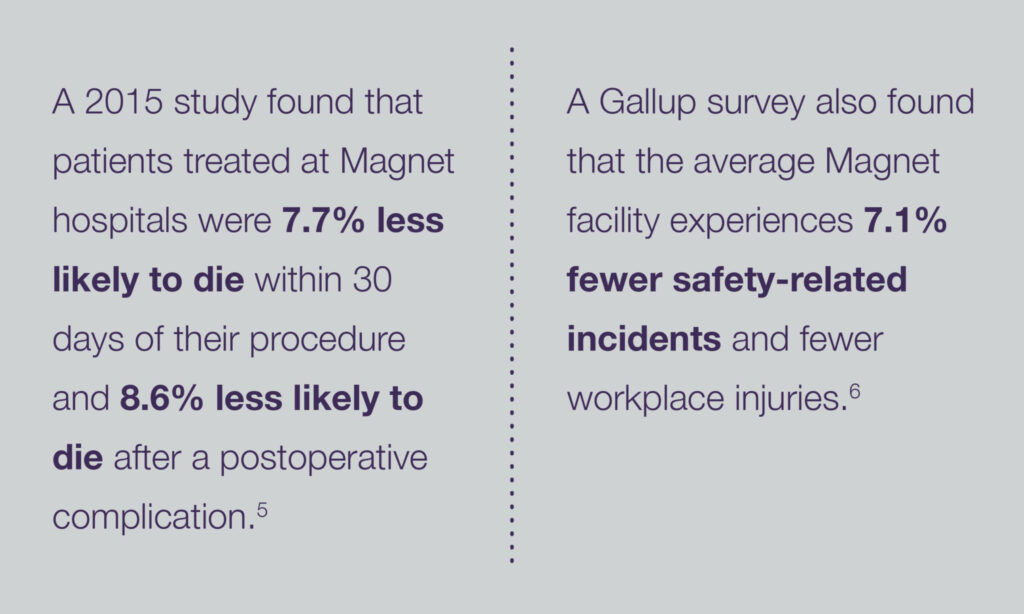
The benefits of driving down sentinel events with technology are obvious—less patient harm, more peace of mind for staff, and less legal and financial liability. But beyond that, executives should also consider how focusing on innovation that enhances communication can improve patient care, which in turn can boost performance rates that lead to better outcomes for all involved. Improved patient outcomes have been linked to higher rates of nurse engagement,4 meaning communication solutions that promote higher levels of engagement are likely to foster an environment for better care. What’s more, higher levels of nurse engagement are also linked to hospitals with increased achievement statuses, including the well-known Magnet designation.5 Magnet hospitals are noted for innovations in nursing practice, superior work environments, and quality patient outcomes, among other benchmarks.5 To be clear, having advanced technology isn’t the only hallmark of a typical Magnet facility, but it can be the rising tide that lifts all boats. When you equip your staff with tools that make them more effective and efficient, the downstream benefits are almost limitless.
Sentinel events aren’t a secret or a new phenomenon—health systems do their level best to avoid them every day. But as awareness and usage of clinical communication solutions have risen in the past decade, it’s become apparent that this technology—which enables communication and collaboration across the entire care team—needs to be part of any integrated patient safety strategy.
By shortening communication cycle times, reducing alert and alarm fatigue, and giving clinicians a structured and intuitive way to coordinate patient care in real time, these solutions can alleviate many of the root causes that contribute to sentinel events.
If you’d like to learn more about unified healthcare communication and how it can help your organization reduce variation and risk while improving quality, contact us today.
1 Sentinel Events, The Joint Commission, 2022: https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/
2 10 Most Common Sentinel Events of 2021: Joint Commission, Becker’s Hospital Review, Feb. 22, 2022: https://www.beckershospitalreview.com/patient-safety-outcomes/10-most-common-sentinel-events-of-2021-joint-commission.html
3 Alarm Fatigue: A Patient Safety Concern, American Association of Critical-Care Nurses (AACN) Advanced Critical Care, Sue Sendelbach, RN, PhD, CCNS and Marjorie Funk, RN, PhD, Oct. 2013: acnjournals.org/aacnacconline/article-abstract/24/4/378/14745/Alarm-FatigueA-Patient-Safety-Concern
4 What is a Magnet Hospital? Southern New Hampshire University, 2021: https://www.snhu.edu/about-us/newsroom/health/what-is-a-magnet-hospital
5 Hospitals In ‘Magnet’ Program Show Better Patient Outcomes On Mortality Measures Compared To Non-‘Magnet’ Hospitals, National Library of Medicine, June 1, 2016: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462174/
6 Going for the gold: The value of attaining Magnet Recognition, MyAmericanNurse.com: https://www.myamericannurse.com/going-for-the-gold-the-value-of-attaining-magnet-recognition/