Healthcare Communication Software: History and Future Predictions
TABLE OF CONTENTS

Hospitals rely on hundreds of technology systems for care delivery and communication. But before software, the internet, and AI, healthcare—and the need for critical communication—still existed. So, when did these systems emerge, and how did they shape modern healthcare communication?
Let’s explore key milestones in provider and patient communication and what’s next for healthcare communication software.
Healthcare Communication Before the Digital Era
Before digital tools, hospitals used basic methods like chalkboards, paper notes, and face-to-face conversations to communicate about patient care. While this worked, it often led to miscommunication and care delays, which impacted patient outcomes.
“The goal of hospital communication systems is to allow for accurate and efficient communications and advances in technology have been used to achieve this goal.”
—National Library of Medicine
Before the internet, tools like landline phones, intercom systems, and hospital switchboards helped speed up communication. By the 1980s, pagers had become common in hospitals worldwide.2 Although pagers made doctors more accessible, many physicians found them disruptive, and as the volume of “urgent” messages increased, response times often slowed.3 Not ideal for timely care!
The need to get information to the right provider quickly has always been critical. In fact, communication failures contribute to 27% of medical malpractice cases.4 If you don’t know which care team member to contact or how—maybe because of an outdated schedule—it becomes hard to reach the right person quickly. That can absolutely impact patient outcomes.
Hospitals often used paper schedules or Gantt charts to track provider availability and patient appointments. But these static methods couldn’t keep up with the complex, real-time needs of care teams.
For instance, if Dr. Martinez was called into emergency surgery, the paper schedule wouldn’t reflect her new location, leaving the team in the dark. Hospital switchboard operators also struggled with outdated schedules, making it difficult to connect callers to the right clinician.
Why Healthcare Communication Moved to Digital Tools
Digital tools have had a major impact on healthcare, and a few stand out. Fax machines, introduced in the late 1960s,5 became widely used by the 80s and 90s. They allowed staff to quickly share lab results, schedules, and patient data without needing a phone or pager. Faxing took about a minute and made it possible to send copies worldwide,6 but it posed risks—data could be intercepted or sent to the wrong number.7
The introduction of personal computers, and later the electronic health record (EHR), revolutionized healthcare. Early EHRs organized patient data for easy access, categorized by date or service type. By the mid-2000s, EHRs became essential for healthcare communication.8
The internet’s arrival in the 80s further changed the communication landscape. Email and other messaging systems appeared, but safety concerns over patient data sharing quickly surfaced. Despite these advances, most hospitals still relied on landlines, pagers, and fax machines, which led to slow communication and delayed care.
A turning point came with the Health Insurance Portability and Accountability Act (HIPAA) in 1996, setting national standards for protecting patient health information (PHI).9 Before HIPAA, PHI was often stored in physical file cabinets and faxed, causing delays that could affect emergency care.
“The HIPAA security rule complements the privacy rule and requires entities to implement physical, technical, and administrative safeguards to protect the privacy of PHI.”
—Journal of Nuclear Medicine Technology
In 2009, the HITECH Act pushed for widespread EHR adoption, aiming to integrate medical data for both providers and patients. It also increased penalties for HIPAA violations,9,10 raising the bar for secure healthcare communication.
Healthcare Communication and Scheduling: Connecting the Dots
From the late 80s to the 2000s, rapid advances in technology—along with pressure from HIPAA and the HITECH Act—pushed clinical communication forward. Cell phones, tablets, and smartphones became common in healthcare, and many EHRs today are accessible on mobile devices. However, some don’t fully support communication software integrations, forcing clinicians to juggle multiple apps and tabs while managing patient data.
Communication is still playing catch up. Though many care teams use some kind of communication platform today, it wasn’t until 2024 that the Centers for Medicare & Medicaid Services (CMS) began allowing hospitals to text orders using secure messaging platforms. The Joint Commission followed suit soon after, stating that “accredited healthcare organizations that implement a secure texting platform (STP) may text patient information and orders to members of the care team.”11 The slow adoption of better communication tools is often due to poor integration with scheduling, which makes it hard to reach the right provider quickly.
Scheduling technology has also evolved in the healthcare space. Starting in the 1950s, algorithms helped speed up scheduling decisions.12 These heuristic models generated quick, acceptable shift schedules, but the outcomes weren’t always optimal. With “good enough” schedules, problems usually pop up—gaps in coverage can leave care teams struggling to keep up, and uneven shift allocation can contribute to provider burnout.
In the early 2000s, combinatorial optimization ushered in a more advanced approach, boasting the ability to create gap-free schedules that accounted for a seemingly limitless number of variables in real time. The aviation industry and even Major League Baseball rely on this technology to handle complex scheduling needs, leaning into its ability to account for specific factors like stadium capacity, flight duration, game length, and aircraft weight limits. In healthcare, this technology has enabled schedulers to more effectively manage provider availability, patient demand, clinician preferences, operating room access, and countless other variables—all in real time.
Combinatorial Optimization vs Heuristics
Goal
Outcome
Time Required
Combinatorial
Optimization
Finds optimal solution to a problem
Can guarantee the optimal solution (or how close it is to the optimal solution)
Works to find the best solution possible in a matter of minutes
Heuristic
Scheduling
Generally finds non-optimal solutions to problems
Cannot guarantee the optimal solution (or how close it is to the optimal solution)
Usually runs fast
Let’s go back to Dr. Martinez. When a scheduler uses a digital solution to plan schedules months ahead, the goal is to make sure all clinicians know their shifts—clinic, call, and OR—well in advance. When Dr. Martinez learns she’s pregnant, her schedule needs to be adjusted. In the few months before delivery, she’ll require lighter shifts, and once the baby arrives, she’ll need to be removed from the schedule entirely for a two-month maternity leave.
With technology that uses combinatorial optimization, these changes are seamless. The scheduler can easily assign Dr. Martinez lighter shifts starting in six months. He also sets parameters to remove her from the schedule during her leave and assigns lighter shifts—like morning clinics—when she returns.
The schedule gets updated quickly, and the adjustments are visible to everyone right away. Because the solution in this example is cloud-based, every team member always has access to the latest schedule, making it the single source of truth across the organization. That level of transparency and efficiency makes communication faster, more accurate, and easier for everyone.
The benefits of having a single source of truth for schedules extend beyond availability. Today’s secure messaging systems can escalate messages when clinicians don’t respond quickly, but without accurate schedules, messages may be sent to the wrong person.
Patient Engagement Tools: A Brief History
Patients used to rely on letters and phone calls to reach their providers, limiting both accessibility and timeliness. Letters could get lost, and missed reminder calls might lead to missed appointments. These communication barriers often left patients in the dark, contributing to lower engagement rates.
Engaged patients tend to experience better health outcomes,13 which is why tech advancements have aimed to strengthen these patient-provider connections. The early 90s and 2000s saw the introduction of patient portals,14 but they required computer access and login credentials. Plus, portal-based communication was often slow, leaving patients waiting too long for important answers.
Many organizations still struggle to manage after-hours patient calls and care. Since their introduction in the 1960s,15 call centers and hospital switchboards16 have been used to route calls between patients and providers. They often fall short when it comes to managing on-call coverage. The missing piece? The lack of real-time schedule accuracy. Imagine a patient navigating a lengthy voicemail tree only to have their urgent call go unanswered because the schedule isn’t right.
This is why healthcare leaders now see digital schedules as a much-needed single source of truth, especially when paired with escalation processes that prevent communications from falling through the cracks. These escalation policies contribute to timelier care, particularly after hours.
And then there’s the pandemic, which caused patient expectations to shift. As a result, telehealth has exploded in the past four-plus years.
Today, hundreds of apps allow patients to access their medical records, chat with providers, and even jump on video calls—all from their phones. Patients who struggle with transportation or mobility can now receive care from home. Prescription refill requests, appointment reminders, and communication with doctors can happen via text, making the entire process much more convenient.
These innovations have empowered patients to engage more actively with their care. But could communication be even faster and more seamless? When healthcare systems adopt interconnected communication platforms, the answer is yes.
Unifying Platforms for Providers and Patients
With advancements in healthcare communication, it’s easier than ever for providers and patients to stay connected. Since patients often receive care at multiple locations, it’s crucial that their health information (PHI) can move seamlessly between them. Unified healthcare platforms make this possible by integrating patient records, provider collaboration, and communication tools in one system.
For example, care teams can now communicate directly within the EHR—no switching between different apps to relay important information. This allows them to share patient data in a HIPAA-compliant manner. If a clinician isn’t sure who to contact, they can typically search by role to find the right person.
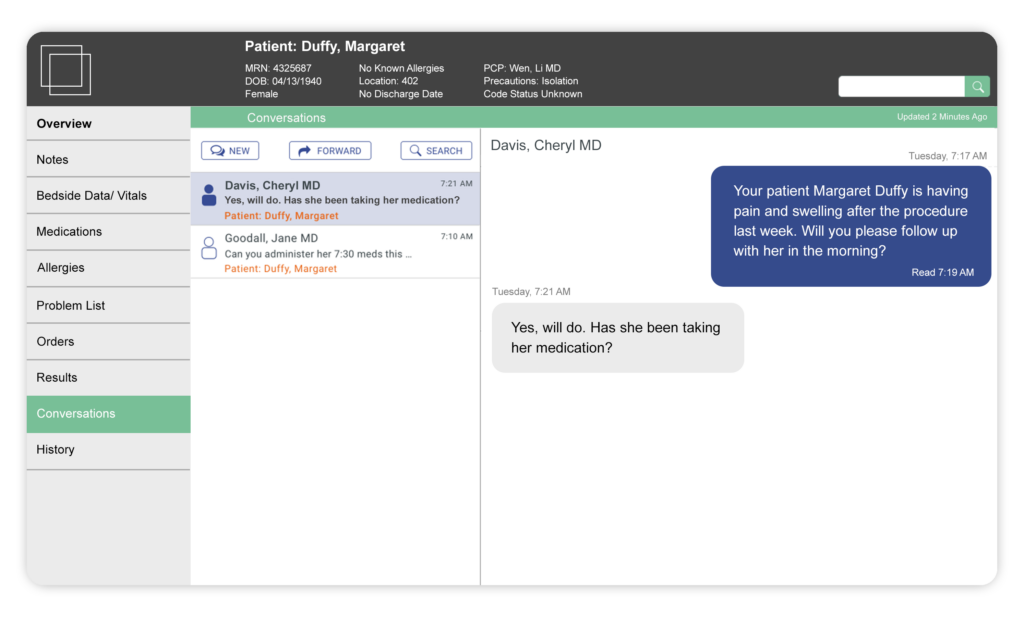
Imagine Dr. Martinez is at her clinic and her patient, Cynthia, is experiencing respiratory distress. Dr. Martinez needs to consult the respiratory therapist but doesn’t know who’s on call. She opens Cynthia’s file in the EHR, types “respiratory therapist on call,” and sees Dr. Wilson is available. She quickly sends a message and includes José, the nurse who helped with Cynthia’s intake, so the entire care team is looped in. Dr. Wilson receives the message and can see all relevant information about Cynthia with just a few clicks. In minutes, he’s on his way to help.
Patients like Cynthia are involved too. She can access her information through the EHR, and José can send a secure follow-up message to her phone, reminding her to pick up a prescription. If Cynthia needs further help, she can even use the same platform to have a video chat with her care team.
Healthcare AI Tools: What’s Next for Healthcare Communication?
As interoperability improves, the next big step in healthcare communication will involve more closely integrating artificial intelligence (AI). AI tools will likely be used to enhance secure messaging, from AI-assisted message composition to automated order placement and even spell-checking of medical terminology. These advancements will help to ensure messages are clear and complete from the start, reducing back-and-forth communication and speeding up care coordination.
Potential AI Use Cases in Healthcare
The possibilities seem endless with AI, but here are a few ways it might exert its power in the healthcare communication and scheduling space:
- Natural language queries for data reporting: AI could help generate custom reports based on healthcare communication data, such as number of messages sent and response times. A user could ask, “Show me all critical results delivered to our hospitalist team last month, organized by provider, day of the week, and response time.”
- Generative AI for message composition & order submission: AI could assist in writing messages or placing orders by offering text suggestions, checking the accuracy of medical terminology, or prompting providers for specific details like medication dosage and frequency.
- Natural language message processing: For secure communication, AI could allow a messaging platform to automatically detect certain user responses (e.g., “OK” or “Thanks”) to prevent message notification and escalation policies from being triggered. This would alleviate instances of providers being distracted by noncritical communications.
- Predictive scheduling: AI could analyze historical data to suggest shift swaps and other schedule details, making scheduling faster and more in tune with true organizational needs.
- Language-based IVR: In after-hours and transfer center communication solutions, AI could allow callers to use natural language to explain their reason for calling rather than asking them to answer a predetermined—and not always relevant—list of questions.
- Predictive communication routing: To speed up delivery and response times, AI could help providers by automatically determining the best communication pathway based on the contents of their message.
Wearables and Remote Monitoring

Wearables and remote monitoring can significantly cut communication cycle times by eliminating waits for lab or test results. When paired with AI, these devices can send targeted notifications to care team members. For example, a wearable heart monitor could alert the on-call cardiologist if a patient’s heart rate is elevated for too long.
These granular use cases highlight the concept of the “real-time health system,” which Gartner defines as “a technology and operational archetype for the next generation of hospitals and health systems.” Gartner believes clinical communication systems “enhance care team effectiveness, optimize nursing operations, and reduce toil” while improving “situational awareness surrounding the patient and information sharing at the point of care and during care transitions.”16
Modern healthcare communication tools are key catalysts for making this vision a reality because they can turn a hospital full of siloed departments into an interconnected site of care, readily distributing the most important information to the people who need to act on it.
Interoperability
Achieving interoperability across health IT solutions is another key industry goal. Seamless communication between systems enhances collaboration, patient care, and results sharing and leads to smoother care delivery.
However, true interoperability is challenging to achieve, especially when connecting older systems like on-prem call center technology with newer, cloud-based software. But here again, AI offers some new opportunities. AI can enhance interoperability through:
- Data standardization and normalization: AI can analyze and convert various data formats into standardized forms (e.g., HL7, FHIR), allowing systems like EHRs and lab software to communicate effectively.
- Intelligent data mapping: AI can match data fields across different systems, ensuring accurate information exchange even when labels differ (e.g., “Physician” vs. “Provider”).
- AI-driven decision support tools: AI can aggregate data from multiple sources to provide clinicians with actionable insights, improving decision-making at the point of care.
- Personalized patient communication and scheduling: AI can automate and personalize patient interactions, sending appointment reminders and follow-up instructions.
Data Security
While AI isn’t inherently HIPAA-compliant, it can be designed to meet HIPAA regulations.18 By programming AI systems to adhere to safeguards, AI can enhance data security in healthcare communication.
For example, AI can detect anomalies and flag unusual activities (like unauthorized edits or access attempts) while quickly alerting security teams.
Additionally, AI can help ensure compliance by monitoring communication tools for HIPAA adherence. This proactive approach can save health systems money by preventing costly violations, which can range from hundreds of dollars to nearly $2 million apiece, depending on the infraction.19
Technology’s Role in Shaping Healthcare’s Future
Healthcare communication has transitioned from basic methods to sophisticated, interconnected digital platforms. Each advancement faced unique challenges, yet each step brought us closer to today’s efficient, secure, and patient-centered communication standards. Key points to remember:
- Evolution of Communication Tools: From chalkboards and pagers to EHRs and secure messaging platforms, every innovation in healthcare communication aims to deliver faster, more accurate information exchange.
- Regulatory Impact: The adoption of EHRs and HIPAA regulations established critical standards for patient data privacy, security, and reliability, laying the foundation for secure communication practices.
- Scheduling Integration: Combining communication and scheduling tools has streamlined workflows and improved care coordination, allowing messages to reach the right person at the right time, which optimizes patient care.
- AI and Future Innovation: As AI integrates more deeply into healthcare, it will enhance message delivery, boost scheduling accuracy, strengthen data security, and support interoperability across IT systems.
- Real-Time Health Systems: By embracing innovation and focusing on interoperability, healthcare can move towards real-time, seamless communication that enhances both patient and provider experiences.
Looking ahead, ongoing advancements in AI and interoperability will continue to shape healthcare communication, making the vision of a “real-time health system” increasingly achievable.
Sources:
- 1,3: The hospital pager: Out with the old or here to stay? National Library of Medicine: https://pmc.ncbi.nlm.nih.gov/articles/PMC6490267/#:~:text=The%201950s%20saw%20the%20advent,pagers%20equipped%20with%20small%20keyboards.
- 2: History of Pagers and Beepers. ThoughtCo.Com: https://www.thoughtco.com/history-of-pagers-and-beepers-1992315#:~:text=The%20First%20Pagers,%2C%20firefighters%2C%20and%20medical%20professionals.
- 4: Poor communication by health care professionals may lead to life-threatening complications: examples from two case reports. National Library of Medicine: https://pmc.ncbi.nlm.nih.gov/articles/PMC6694717/
- 5: When was the Fax Machine Invented? HP.com: https://www.hp.com/us-en/shop/tech-takes/when-was-fax-invented#:~:text=The%20first%20recognizable%20version%20of,their%20products%20to%20do%20more.
- 6,7: The History of the Fax Machine. Vyne Medical: https://vynemedical.com/blog/the-history-of-the-fax-machine/
- 8: What Is an EMR? All You Need to Know About Electronic Medical Records. SigmaMD: https://sigmamd.com/blog/emr#:~:text=EMRs%20organize%20data%20in%20a,service%2C%20or%20other%20relevant%20criteria.
- 9,10: Review of HIPAA, Part 1: History, Protected Health Information, and Privacy and Security Rules. Journal of Nuclear Medicine Technology: https://tech.snmjournals.org/content/47/4/269#:~:text=care%20(6).-,NEW%20RULES,Act%20in%202009%20(7).
- 10: HIPAA Turns 10: Analyzing the Past, Present, and Future Impact. George Washington University Law School: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2245022
- 11: Use of secure text messaging for patient information and orders. The Joint Commission: https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/joint-commission-online/june-5-2024/use-of-secure-text-messaging-for-patient-information-and-orders/
- 12: A brief history of heuristics: how did research on heuristics evolve? Nature.com: https://www.nature.com/articles/s41599-023-01542-z
- 13: Impact of Patient Engagement on Healthcare Quality: A Scoping Review. National Library of Medicine: https://pmc.ncbi.nlm.nih.gov/articles/PMC9483965/
- 14: Patient Portals and Patient Engagement: A State of the Science Review. National Library of Medicine: https://pmc.ncbi.nlm.nih.gov/articles/PMC4526960/#:~:text=Patient%20portals%20were%20introduced%20and,)%20%5B3%2C4%5D.
- 15: The History of Call Center Services. ROI CX Solutions:https://roicallcentersolutions.com/blog/the-history-of-call-center-services/
- 16: The Rise and Fall of Telephone Operators. History.com: https://www.history.com/news/rise-fall-telephone-switchboard-operators
- 17: Magic Quadrant for Clinical Communication and Collaboration. Gartner, Barry Runyon, 31 July 2023.
- 18: AI Chatbots and Challenges of HIPAA Compliance for AI Developers and Vendors. National Library of Medicine: https://pmc.ncbi.nlm.nih.gov/articles/PMC10937180/
- 19: What are the penalties for violating HIPAA? American Dental Association: https://www.ada.org/resources/practice/legal-and-regulatory/hipaa/penalties-for-violating-hipaa