Event
Why Integrations Matter for Clinical Communication
Watch NowTABLE OF CONTENTS

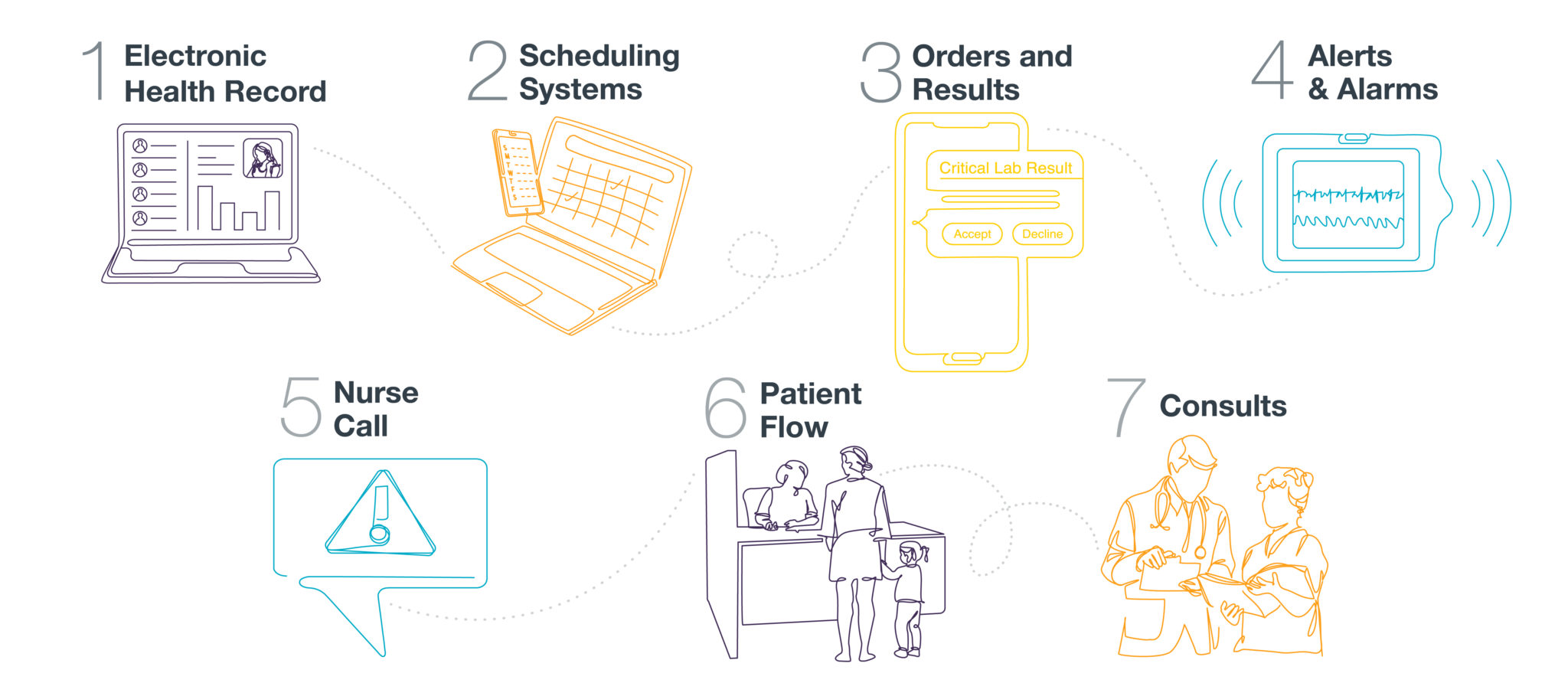
Good clinical communication is at the heart of better care and higher satisfaction for patients and providers. Clinical communication solutions that integrate with EHRs, scheduling software, and systems that deliver important alerts & alarms create more robust communication pathways, which helps to accelerate speed to care and streamline care coordination.
Finding the right communication solution that tightly integrates with your organization’s clinical, IT, and telecom systems will lead to quicker, more error-free communication. Here are several key clinical integrations that enhance collaboration workflows for the care team and should serve as the foundation of any clinical communication blueprint.
Electronic health records (EHRs) are an integral part of the care delivery process for nearly every health system, and they contain everything from patient medical history, diagnoses, and medications to treatment plans, immunization dates, allergies, and laboratory and test results. They are intended to provide a broad view of a patient’s care while making relevant information readily available to authorized members of the care team.
Unfortunately, clinicians waste countless hours on redundant EHR activities like logging in, finding available workstations, checking the status of test results, searching for care team members, and taking clinical notes. By integrating a clinical communication system with your EHR, many of these activities can be accomplished quickly and easily from a mobile device. With this integration, the right communication solution will allow clinicians to:
With more advanced integrations, the clinical communication solution can also be embedded directly within the EHR to promote even greater efficiency.
An integrated scheduling system is a powerful component of the enhanced clinical collaboration platform that improves provider satisfaction, enhances speed to care, and saves valuable time for the care team. An integrated schedule grants accurate visibility of every on-call physician, ensuring messages are delivered to the right provider at the right time. Having this information at the click of a mouse is essential for efficient provider communication, as clinicians often waste valuable time looking up other clinician information, verifying call schedules, and tracking down the appropriate care team member.
An integrated schedule improves operational efficiencies by ensuring the following:
Some communication platforms do offer native on-call scheduling functionality, and for those that don’t, they should always be able to integrate with third-party scheduling solutions. For organizations with more complex scheduling needs, solutions that auto-generate schedules based on rules and provider preferences are available.
Though EHR integration was covered up top, it’s worth mentioning again in the context of orders and results. Orders are, of course, managed in the EHR, while information about test results comes from the laboratory information system (LIS).
Integrating with these two systems helps clinicians to provide more efficient patient care by instantly delivering critical orders and test results and eliminating the need to return to the workstation for updates. The most advanced clinical communication solutions also have intelligent routing that can auto-escalate time-sensitive orders or abnormal test results that remain unactioned after a predetermined amount of time. This helps to prevent patient harm/sentinel events by ensuring that the most important information related to patient care doesn’t fall through the cracks.
Clinicians are frequently inundated with calls, beeps, bings, buzzes, and other patient alert notification sounds throughout their shifts, and it’s an understatement to say that this information can be difficult to process accurately and efficiently. To make matters worse, recent research indicates that anywhere from 80% to 99% of patient alarms are “false or clinically insignificant and do not represent real danger for patients, leading caregivers to miss relevant alarms that might indicate significant harmful events.”1
Integrating your clinical communication system with alerts & alarms from biomedical devices, physiological monitors, and other systems allows the care team to oversee patients in real time by remotely assessing alarms to ensure the most critical ones are spotted more quickly. This also reduces the aforementioned alarm fatigue for clinicians and alleviates patient dissatisfaction related to hospital noise levels.
By integrating a nurse call system with a clinical communication platform, all nurse call alarms can be sent directly to mobile users in a way that allows urgent calls to be distinguished from lower priority calls like water requests. These alarms can be shared or forwarded within the care team, and critical alarms can be escalated if they’re not acted upon within an appropriate time frame.
The ability to answer, prioritize, and assign nurse call alarms from a mobile device unlocks a new level of efficiency within the hospital and reduces repeated and unnecessary trips to patient rooms. By helping nurses to structure, make sense of, and easily respond to the many alarms that are triggered throughout a shift, the nurse call integration allows them to practice at the top of their licensure and focus on the most critical patient care tasks.
Integrating with the admission, discharge, and transfer (ADT) system allows your clinical communication platform to become a secure conduit that automatically sends information about patient transition events to the extended care team, including primary care providers, care coordinators, hospitalists, and others. Patient flow events might include:
This integration closes communication gaps, facilitates patient care collaboration, and can help your organization to meet regulatory requirements.2
Like several other patient care processes, consults tend to require a fair amount of manual babysitting—it’s often necessary to wait for confirmation that the intended physician both received the consult request and will see the patient in a timely manner. In some cases, the request lands in the provider’s EHR inbox, but other workflows may send the request to a group or specialty, at which point it likely has to be triaged by someone like a unit secretary or practice manager. The message may circulate through different parties, and the provider may end up getting repeated communications about the same consult. If the intended provider doesn’t get the request—or needs to hand it off to another provider due to a shift change—the consult request can easily get lost in the fray, causing delays that are almost always detrimental to patient care.
A clinical communication platform with intelligent routing capabilities can be used to automate consult order notifications via integration, including the ability to deliver orders based on priorities like “routine” or “STAT.” This especially saves time for nursing staff and lowers the risk of delayed or missed consults that negatively impact patient care and length of stay.
In their infancy, clinical communication platforms provided much-needed security guardrails for messages containing sensitive patient information. They still play that role today, but the size and scope of their potential impact has grown significantly over time, and much of this growth can be attributed to integrations or, speaking more broadly, efforts related to interoperability.
By ingesting information from other clinical, IT, and telecom systems and distributing it to care team members in a reliable, accurate, and efficient way, deeply integrated clinical communication platforms now play a central role in facilitating timely, high-quality care delivery.
With more than 200 supported integrations, PerfectServe is well equipped to unify communications and streamline care coordination for almost any healthcare facility, large or small. If you’d like to learn how PerfectServe Clinical Communication can transform clinical workflows at your organization, schedule a demo below.
1 Detecting False Alarms by Analyzing Alarm-Context Information: Algorithm Development and Validation, NCBI, May 2020: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7270842/
2 Interoperability and Patient Access Rule- Admission, Discharge, and Transfer Notifications for Hospitals, Psychiatric Hospitals, and Critical Access Hospitals (CAHs) Interpretive Guidance, Centers for Medicare & Medicaid Services, 2021: https://www.cms.gov/medicareprovider-enrollment-and-certificationsurveycertificationgeninfopolicy-and-memos-states-and/advance-copy-interoperability-and-patient-access-rule-admission-discharge-and-transfer-notifications-0
